Treating cancer before 3pm could help patients live longer
Administering cancer treatments at a particular time could be a relatively simple but effective intervention Kenneth K. Lam/ZUMA Press/Alamy
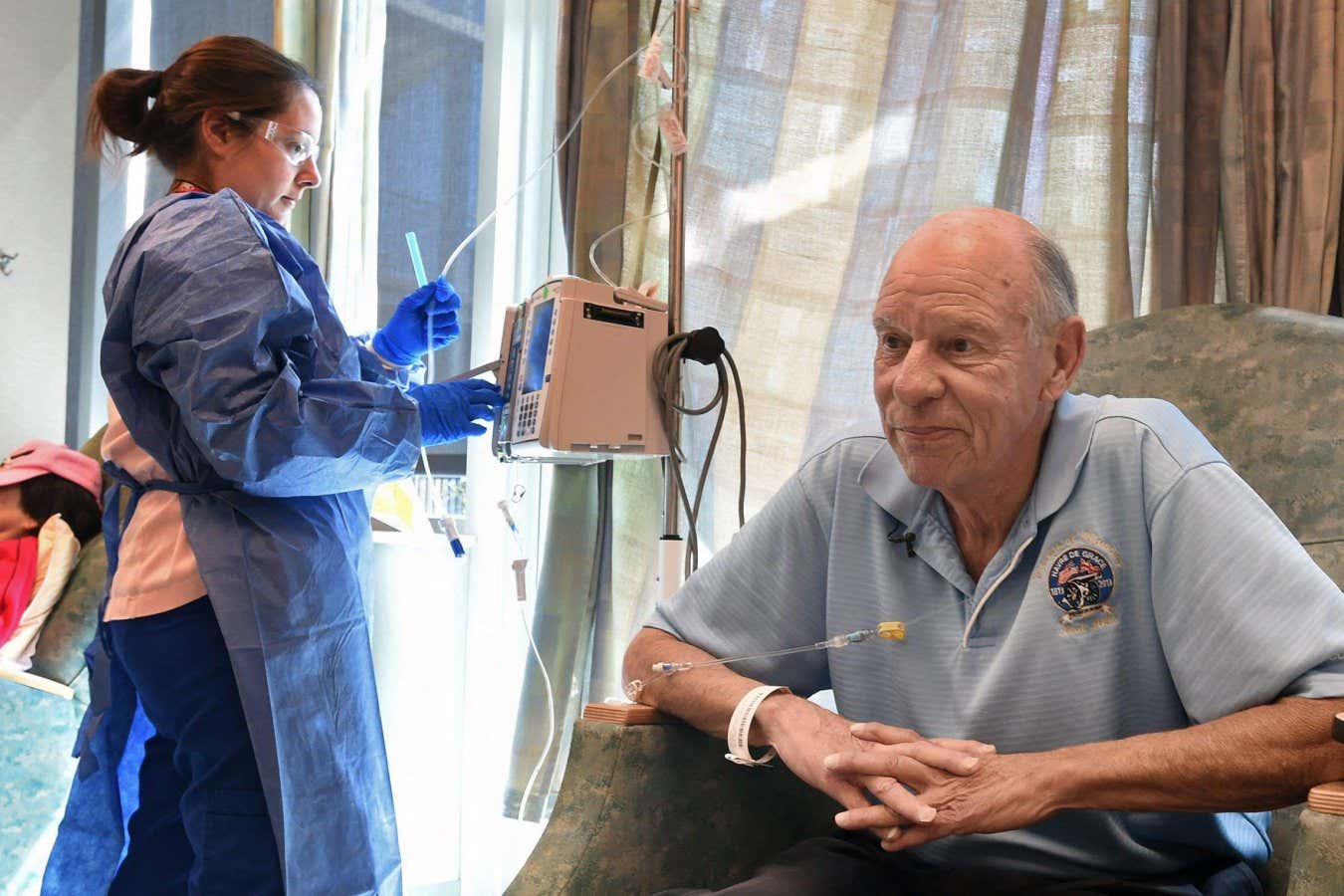
Administering cancer treatments at a particular time could be a relatively simple but effective intervention
Kenneth K. Lam/ZUMA Press/Alamy
Delivering cancer immunotherapy earlier in the day really could extend survival, according to the first randomised-controlled trial into how the timing of such interventions affects patient outcomes.
Our body’s cells and tissues follow 24-hour cycles of activity, known as circadian rhythms, that influence everything from our mood to our metabolism and immune system.
More than a dozen observational studies have found that cancer patients who happen to receive checkpoint inhibitors – a kind of immunotherapy drug that helps certain immune cells kill cancer – earlier in the day seem to have a substantially lower risk of their condition worsening and leading to death.
But now, Francis Lévi at Paris-Saclay University in France and his colleagues have carried out the first randomised-controlled trial into chronotherapy – timing treatments around circadian rhythms – using a combination of chemotherapy and immunotherapy drugs for cancer.
The team recruited 210 people with non-small cell lung cancer who all received four doses of pembrolizumab or sintilimab, two checkpoint inhibitors that work in the same way.
Every three weeks, half of the participants were given a dose before 3pm, while the rest had it later in the day. Shortly after each immunotherapy dose, they all received chemotherapy, which kills rapidly dividing cells and is thought to be less affected by chronotherapy than immunotherapy.
These timings were maintained for the first four cycles of their so-called immunochemotherapy. After that, all the participants continued to receive the same drugs until their tumours worsened or until they no longer responded to the treatment, but these weren’t administered at specific times. Prior studies suggest that focusing on the first four cycles is enough to substantially improve survival outcomes, says team member Yongchang Zhang at Central South University in China.
The researchers tracked the participants for 29 months, on average, after their first treatment dose. They found that those who were initially treated before 3pm survived for an average of 28 months, while those initially treated later in the day survived for 17 months, on average. “The effects are absolutely huge,” says Lévi. “It’s a nearly doubling in survival time.”
“If you compare the results to landmark trials where new drugs have been licenced to use, those drugs rarely have this large an effect,” says Pasquale Innominato at the University of Warwick, UK. The design of this study suggests that shifting the timing of cancer therapy really does improve outcomes, he says. “It’s the strongest evidence for causality.”
The benefits may result from the fact that the immune cells that these checkpoint inhibitors target, called T-cells, tend to congregate around tumours in the morning before gradually migrating into the circulatory system later in the day, so when you give the immunotherapy earlier in the day, the T-cells are closer to the tumour and so destroy more of it, says Lévi.
Further work should explore whether delivering cancer therapies at more specific times – such as 11am, rather than within a window of several hours – has further benefits still, says Lévi. Having a wide window would clearly be preferable for busy hospitals, says Innominato.
We also need to uncover whether controlling the timing of the chemoimmunotherapy cycles beyond the first four could bring even bigger benefits, says Lévi. Optimal timings may also vary between individuals, he says, such as those who identify as morning larks or night owls, whose immune systems may fluctuate distinctly throughout the day.
Whether the results apply to different types of cancer is another open question. Innominato expects they would be similar among other tumours that affect the skin and bladder, due to them commonly being treated with immunotherapy. But it is unlikely that tweaking immunotherapy timing will make it work for tumours that don’t usually respond to the intervention, like those affecting the prostate and pancreas, he says.
Topics:






