Injection turns sleeping tumor immune cells into cancer fighters
Tumors in the human body contain immune cells called macrophages that are naturally capable of attacking cancer. However, the
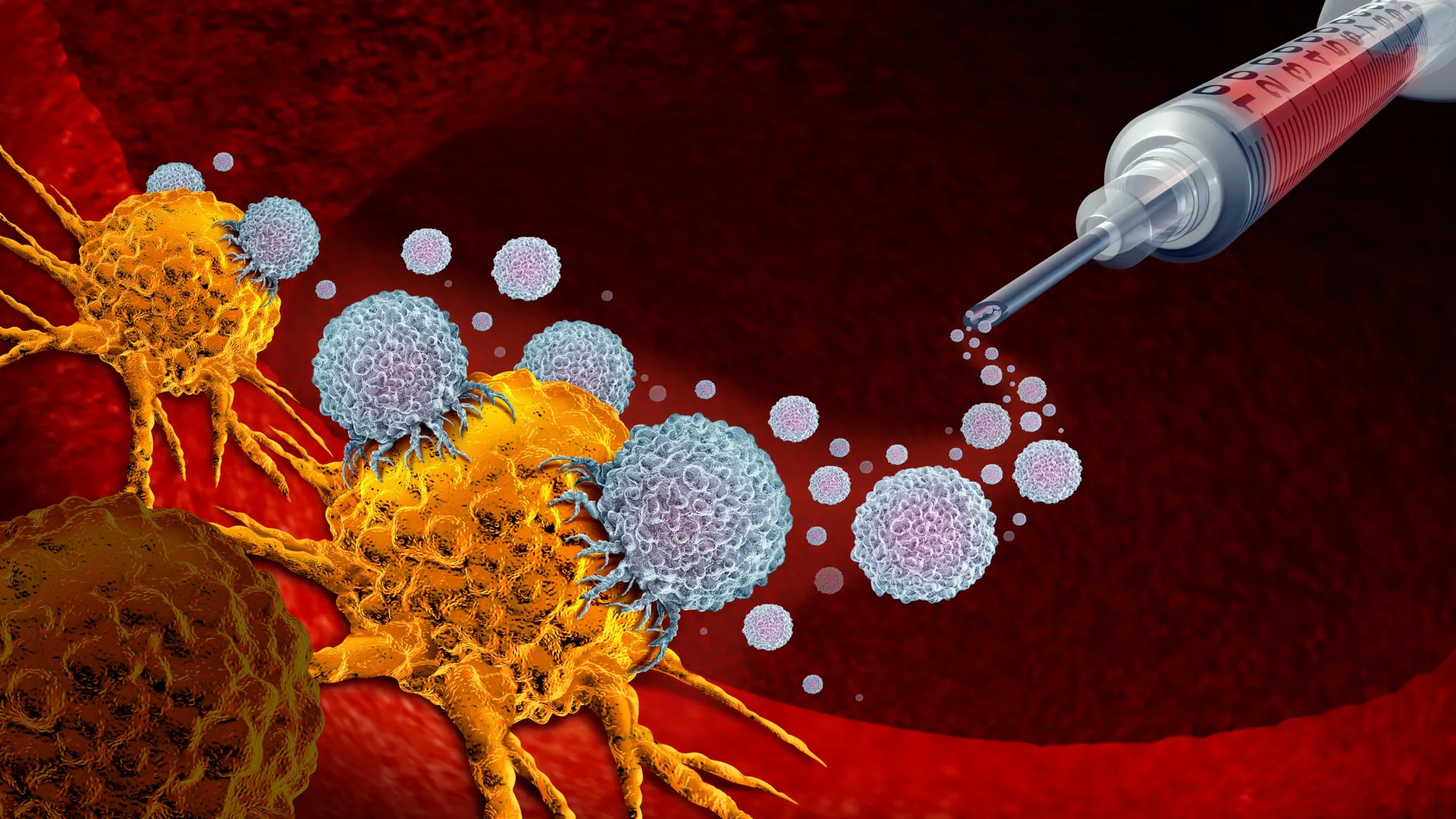
Tumors in the human body contain immune cells called macrophages that are naturally capable of attacking cancer. However, the tumor environment suppresses these cells, preventing them from doing their job. Researchers at KAIST have now found a way to overcome this barrier by directly transforming immune cells already inside tumors into active cancer-fighting therapies.
KAIST (President Kwang Hyung Lee) announced on the 30th that a research team led by Professor Ji-Ho Park from the Department of Bio and Brain Engineering has developed a new treatment approach. When a drug is injected directly into a tumor, macrophages already present in the body absorb the drug and begin producing CAR (a cancer-recognizing device) proteins. This process converts them into anticancer immune cells known as “CAR-macrophages.”
Why Solid Tumors Are So Hard to Treat
Solid tumors — including gastric, lung, and liver cancers — form dense structures that block immune cells from entering or functioning effectively. Because of this physical and biological barrier, many existing immune cell therapies struggle to work well against these types of cancers.
CAR-macrophages have emerged as a promising next-generation immunotherapy. Unlike some immune cells, macrophages can directly engulf and destroy cancer cells. They also stimulate nearby immune cells, helping to amplify the body’s overall anticancer response.
Despite their potential, current CAR-macrophage therapies rely on extracting immune cells from a patient’s blood, growing them in the lab, and genetically modifying them before reinfusion. This process is slow, expensive, and difficult to scale, which limits its practicality for many patients.
Reprogramming Immune Cells Directly Inside the Body
To bypass these challenges, the KAIST team focused on “tumor-associated macrophages” that naturally gather around tumors. The researchers developed a method to reprogram these cells directly inside the body rather than modifying them outside it.
Their approach uses lipid nanoparticles — engineered to be easily taken up by macrophages — loaded with both mRNA that carries cancer-recognition instructions and an immune-activating compound.
As described by the researchers, this method creates CAR-macrophages by “directly converting the body’s own macrophages into anticancer cell therapies inside the body.”
Strong Tumor Suppression in Animal Studies
When the treatment was injected into tumors, macrophages quickly absorbed the nanoparticles and began producing proteins that identify cancer cells. At the same time, immune signaling was activated. The resulting “enhanced CAR-macrophages” showed much stronger cancer-killing ability and stimulated surrounding immune cells, leading to a powerful anticancer response.
In animal models of melanoma (the most dangerous form of skin cancer), tumor growth was significantly reduced. The researchers also found evidence that the immune response could extend beyond the treated tumor, suggesting the potential for broader, body-wide immune protection.
A New Direction for Cancer Immunotherapy
Professor Ji-Ho Park said, “This study presents a new concept of immune cell therapy that generates anticancer immune cells directly inside the patient’s body.” He added that “it is particularly meaningful in that it simultaneously overcomes the key limitations of existing CAR-macrophage therapies — delivery efficiency and the immunosuppressive tumor environment.”
Study Details and Funding
The study was led by Jun-Hee Han, Ph.D., from the Department of Bio and Brain Engineering at KAIST as the first author. The findings were published on November 18 in ACS Nano, an international journal focused on nanotechnology.
The research was supported by the Mid-Career Researcher Program of the National Research Foundation of Korea.






