A simple drug pair may succeed where liver fibrosis treatments failed
Researchers have found that a pair of existing drugs is far more effective when used together than when either
Researchers have found that a pair of existing drugs is far more effective when used together than when either is taken alone. The findings point to a practical and potentially fast route toward a long-awaited treatment for liver fibrosis.
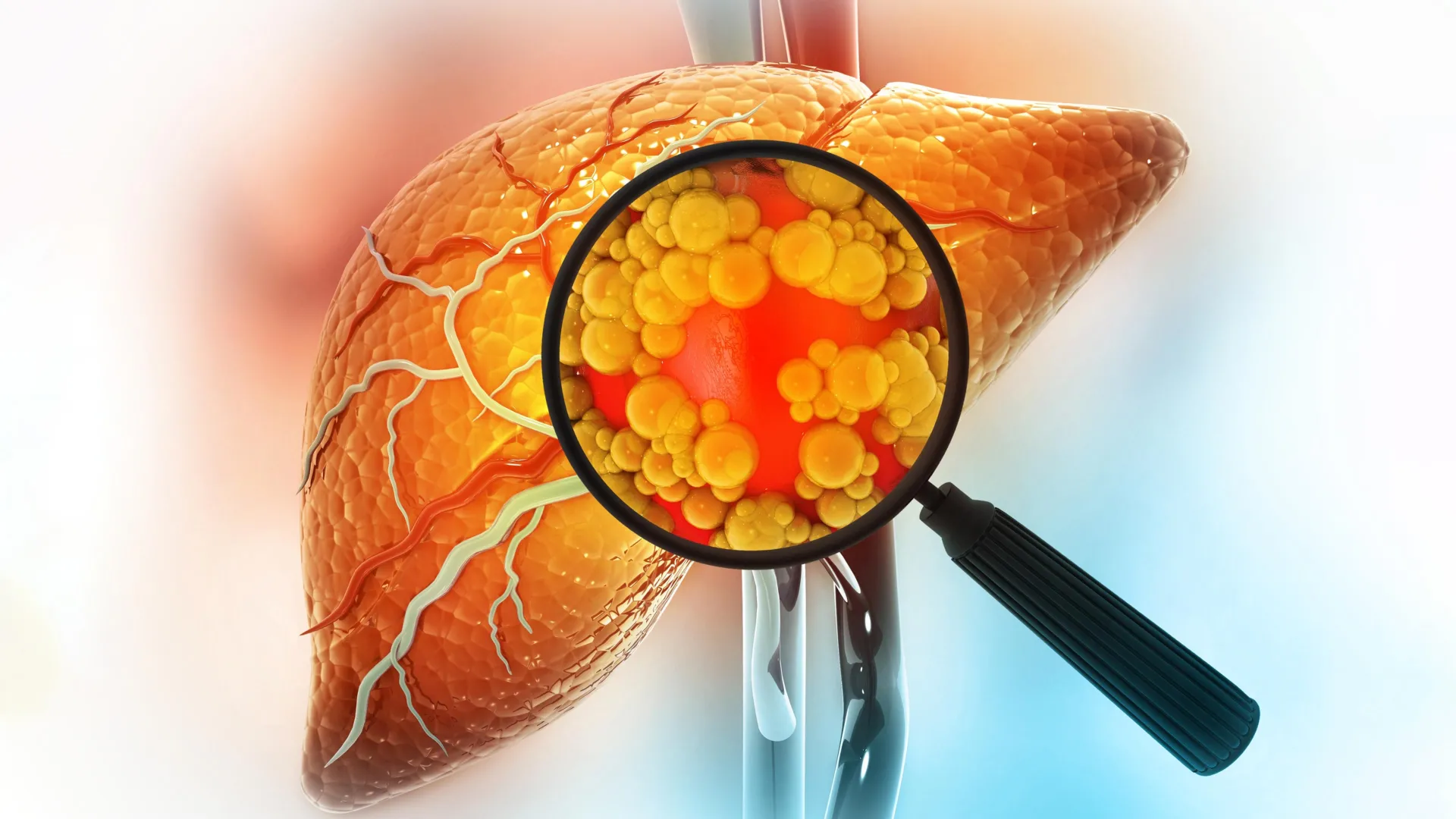
Liver fibrosis is a common but often overlooked condition that affects hundreds of millions of people worldwide. Over time, it can worsen into cirrhosis or liver cancer. Even after decades of scientific effort, there are still no antifibrotic drugs approved for clinical use.
The disease develops when repeated or long-term liver damage — caused by viral hepatitis, excessive alcohol use, metabolic disorders, toxins, or autoimmune disease — triggers an overactive healing response. A major driver of this process is the activation of hepatic stellate cells (HSCs). Under normal conditions, these cells remain inactive. When injury occurs, they switch into collagen-producing cells that build up scar tissue in the liver.
This harmful transformation is controlled by several overlapping signaling systems, including TGF-β, PDGF, and Wnt/β-catenin pathways. Because fibrosis involves many biological routes at once, drugs that target only one pathway often have limited success. This complexity has fueled growing interest in combination treatments that can block multiple drivers of disease at the same time.
A New Use for Two Familiar Drugs
A study published in Targetome on December 15, 2025 by Hong Wang’s & Haiping Hao’s team, China Pharmaceutical University, reports that a fixed-dose combination of silybin and carvedilol can strongly suppress hepatic stellate cell activation. By targeting Wnt4/β-catenin signaling, the drug pair was able to reverse liver fibrosis in experimental models, offering a promising strategy for a disease that currently lacks approved therapies.
To better understand silybin’s potential and its limitations, the researchers combined laboratory experiments, animal studies, phenotype-based drug screening, and molecular analysis. Early tests focused on liver cell injury models triggered by ActD/TNFα, tBHP, and TNFα. These experiments showed that silybin effectively protected liver cells by restoring viability, lowering harmful reactive oxygen species, and reducing inflammatory gene activity. It also showed strong antiapoptotic, antioxidative, and anti-inflammatory effects without detectable toxicity.
However, when researchers examined whether silybin could directly stop fibrosis, the results were less impressive. In human LX-2 and rat HSC-T6 stellate cells stimulated with TGFβ1, silybin only slightly lowered key fibrosis-related markers such as COL1A1, COL1A2, ACTA2, and TGFB. Similar patterns appeared in mice with liver fibrosis caused by carbon tetrachloride exposure. While silybin led to modest improvements in liver enzymes, collagen buildup, and fibrotic gene expression, its benefits appeared to come mainly from protecting liver cells rather than directly blocking stellate cell activation.
Finding the Right Partner Drug
To overcome this limitation, the research team screened 397 FDA-approved drugs using a COL1A1-luciferase reporter system to identify compounds that could enhance silybin’s antifibrotic effect. Carvedilol emerged as the strongest synergistic partner.
When used together, silybin and carvedilol sharply reduced collagen production and stellate cell activation in human and rat cell cultures, as well as in primary hepatic stellate cells. In every case, the combination outperformed either drug on its own.
Further testing in animals showed that a fixed-dose ratio of 50:1 (silybin to carvedilol) produced the most consistent and powerful results. This optimized pairing significantly reduced liver injury, inflammation, and fibrosis severity in mice. The effects increased with dose and were stronger than those seen with obeticholic acid.
How the Drug Duo Stops Liver Scarring
Mechanistic studies revealed why the combination works so well. Together, silybin and carvedilol shut down the Wnt/β-catenin signaling pathway more effectively than either drug alone. This includes suppressing the Wnt ligand Wnt4 and reducing downstream β-catenin activity. These findings provide a clear molecular explanation for the combination’s strong antifibrotic effects.
A Fast Track Toward Clinical Use
The study highlights a realistic treatment strategy based on drug repurposing and carefully designed combination therapy. Both silybin and carvedilol are already widely used in clinical practice, have established safety records, and are low in cost. As a result, their combined use could move quickly into clinical testing and help address a major unmet medical need.
Beyond liver fibrosis, the research also demonstrates how phenotype-based screening can reveal powerful and unexpected drug partnerships that may be hiding in plain sight.
Funding and Support
This work was supported by the Major State Basic Research Development Program of China (2022YFA1303800 and 2021YFA1301300); the National Natural Science Foundation of China (82373946, 82073926, 82321005, 82530122, and 81930109); Major Science and Technology Project of Jiangsu Province (BG2024045); Overseas Expertise Introduction Project for Discipline Innovation (G20582017001); the Project of State Key Laboratory of Natural Medicines, China Pharmaceutical University (SKLNMZZ202402); and the Project Program of Basic Science Research Center Base (Pharmaceutical Science) of Yantai University (P202404).